The Robley Rex VA Medical Center in Louisville provides specialty geriatric care for military veterans 65 and older.
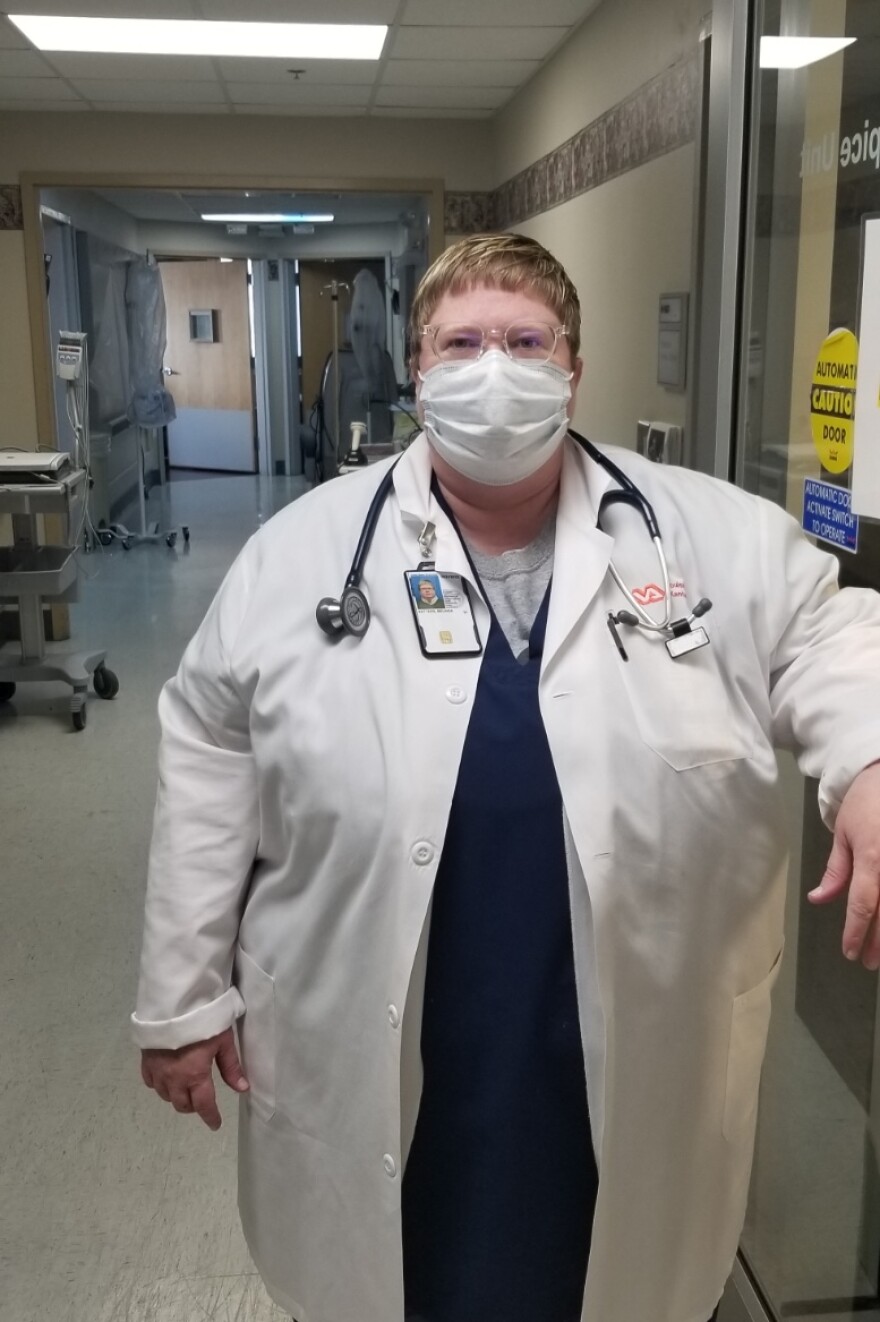
WKU Public Radio reporter Rhonda Miller talked with Director of Inpatient Geriatrics, Dr. Belinda Setters, who says the VA hospital has increased efforts to keep patients active and connected and avoid the negative impacts of isolation, while most visiting is suspended during the COVID-19 pandemic.
Dr. Setters:
So, we take care of the frailest, the oldest folks when they're hospitalized. We actually see patients on all different units, including in the ICU, including in the COVID unit, you know, working in different ways to try to keep the patients engaged and as active as we can, which has been problematic with COVID.
Miller:
What's the general age of the patients you work with?
Dr. Setters:
In general, we usually don't see anyone younger than 65. We prefer 85 and up. And we prefer 85 and up because as a cohort, those patients actually do better with specialized geriatric care. Within that older age group, we found actually that what we call in geriatrics, the “old old,” the 85 and up, especially getting close to the centenarians, actually benefit more from our expertise. And they also tend to have more complications.
Miller:
How has COVID affected the patients you work with physically and emotionally? Do they have visitors?
Dr. Setters:
As a VA facility, we follow the national guidelines. So based on infectious disease recommendations, and so forth, we have not had visitors, for the most part. The exception has been for hospice patients, end of life. We've done everything we can to try to keep people connected. We're using iPads and using FaceTime. We're trying to connect patients with audiovisual as much as we can to let them at least see their family members. That works great for some of the younger patients, for the patients that don't have dementia. What we're finding is that often for dementia patients, it's problematic. They may not understand. They may think they're seeing their loved one, but not really understanding it's not a 3-D person here. And it can get very complicated that way. You layer on top of that macular degeneration, cataracts, low vision as part of aging, hearing impairment, which is a huge issue. And then if they have dementia, which causes cognitive impairment, it becomes extremely difficult for them to connect.

For some patients, the telephone and voice, actually, because they're used to that is a little bit better. In terms of the physical aspect of it, there is a huge fatigue that occurs with COVID that tends to last longer, even after the initial respiratory part of the viral infection is cleared. There's a fatigue and even an anorexia.
Miller:
Anorexia, meaning they don’t eat?
Dr. Setters:
Right, exactly, so they lose appetite. Some of them lose a sense of smell. Some of them have issues with taste. When you look at the medical evidence, the two things that have been consistently shown, especially in older patients to help with outcomes, is good nutrition and activity. Mobility is really important, but the patient has to have the energy to do that.
Miller:
These are the most frail elderly, obviously. Is there anything specific about veterans?
Dr. Setters:
Our veterans are a unique group. Many of them, because they do have special needs, we've heard a lot about depression and suicide risk and recently and that's an absolutely issue we have to look at. But they’re a really giving, generous group of people, and so I feel like we're fortunate to be able to help them. They tend to be very gracious as a group and very thankful and appreciative of care, which makes our job just that much more enjoyable, I guess, and rewarding.
----
Dr. Belinda Setters completed a bachelor's and master's degree in biology from Western Kentucky University and received her medical degree from the University of Louisville. She completed her training with a residency in Internal Medicine and a fellowship in Geriatric Medicine at St. Vincent Hospital and Health Sciences in Indianapolis, an affiliate of Indiana University.
In addition to her position at the Robley Rex VA, she is an Associate Professor of Geriatrics and Palliative Medicine at the University of Louisville. She is currently working to improve care for dementia patients who are un-befriended or did not make important decisions early in hospitalization.